Osteoarthritis (OA) is a widely prevalent and potentially debilitating condition that impacts millions of individuals globally. Understanding the nuances of OA is crucial for early detection, effective management, and maintaining a good quality of life.
Table of Contents
ToggleWhat is Osteoarthritis?
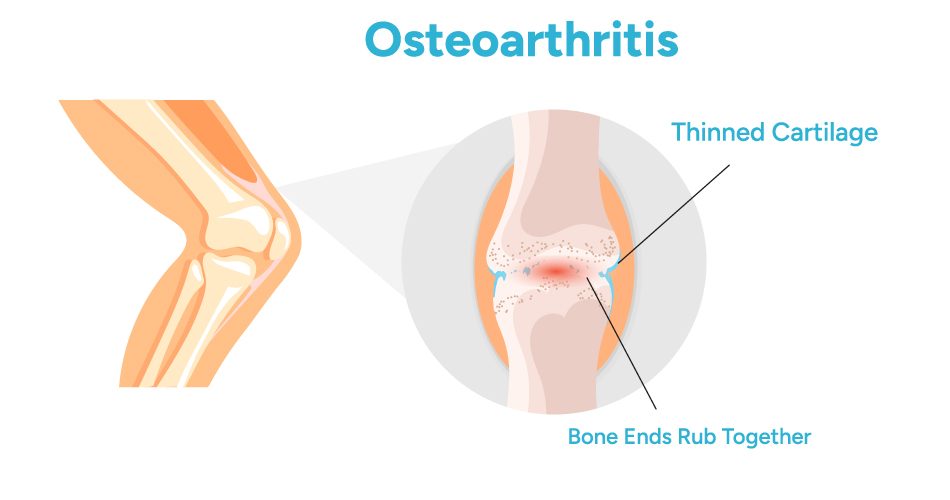
Osteoarthritis (OA) is the most common form of arthritis, It is a degenerative joint disease characterized by the gradual breakdown of cartilage, a firm, rubbery material that covers the ends of bones in normal joints. As cartilage deteriorates, bones begin to rub against each other, leading to pain, stiffness, and reduced mobility. This process can affect any joint in the body, but the most commonly impacted areas include the knees, hips, hands, and spine.
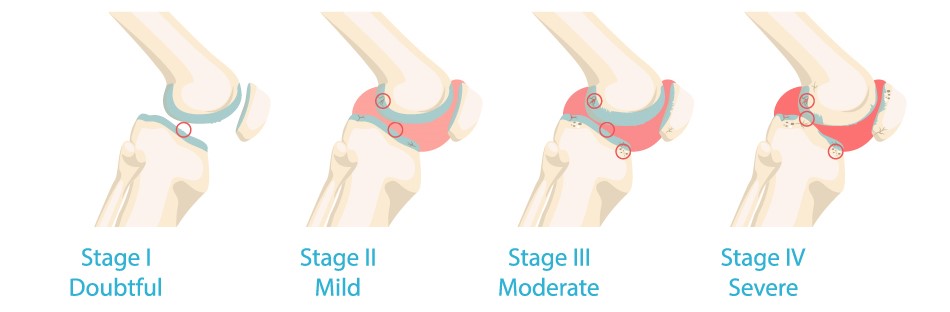
Several Stages of Osteoarthritis
Osteoarthritis Types
There are several types of osteoarthritis, each with its unique characteristics. Understanding these types can provide insights into the progression and management of the condition.
Degenerative Osteoarthritis
Degenerative osteoarthritis is the most common type and occurs due to the natural ageing process. Over time, the wear and tear on joints lead to the breakdown of cartilage. This type is often associated with ageing-related factors, making it imperative for individuals in their senior years to be vigilant about joint health.
Arthritis Osteoarthritis
Arthritis is a broader term encompassing various joint conditions, with osteoarthritis being the most prevalent form. Arthritis osteoarthritis specifically refers to the degeneration of cartilage in joints, resulting in the characteristic symptoms associated with osteoarthritis.
Osteoarthritis Symptoms
Recognizing the symptoms of osteoarthritis is paramount for early intervention and effective management. While symptoms may vary in intensity, common indicators include:
- Joint Pain: Persistent pain in the affected joint, often aggravated by movement
- Stiffness: stiffness in the joints, particularly after periods of inactivity or upon waking in the morning.
- Swelling: Inflammation of the joints can lead to swelling, contributing to the overall discomfort associated with osteoarthritis.
- Reduced Range of Motion: As the condition progresses, individuals may experience a decreased range of motion in the affected joints, impacting day-to-day activities.
Causes of Osteoarthritis
While the precise cause of osteoarthritis remains elusive, several factors contribute to its development. Understanding these causes can shed light on the risk factors associated with the condition.
- Age: The risk of osteoarthritis increases with age as cartilage naturally degenerates over time.
- Joint Injury: Previous joint injuries or complex trauma can lead to the development of osteoarthritis later in life.
- Obesity: Excess body weight puts increased stress on weight-bearing joints, leading to cartilage wear and tear.
- Genetics: There may be a genetic predisposition to osteoarthritis, with certain genes influencing cartilage structure and function.
- Joint Overuse: Repetitive use or overuse of joints in certain occupations or activities can contribute to cartilage breakdown.
- Joint Misalignment: Abnormal joint alignment or structural defects can increase the risk of osteoarthritis.
- Other Health Conditions: Certain metabolic disorders, such as diabetes, and inflammatory conditions, such as rheumatoid arthritis, can also increase the risk of developing osteoarthritis.
Impact on Joints
Osteoarthritis exerts a significant impact on joints, affecting their structure and function in various ways.
- Cartilage Degradation: The gradual breakdown of cartilage leads to bones rubbing against each other, causing pain and stiffness.
- Joint Inflammation: In response to cartilage deterioration, the body may initiate an inflammatory process, contributing to swelling and further joint damage.
- Joint Deformities: Advanced(OA)can result in visible changes to the affected joints, affecting both appearance and function.
- Reduced Range of Motion: Osteoarthritis limits the ability of joints to move freely, impacting daily activities and overall mobility.
Ways to manage and treatments osteoarthritis
Effectively managing osteoarthritis involves a multi-faceted approach, incorporating various strategies to alleviate symptoms and improve joint function.
- Lifestyle Modifications: Adopting a healthy lifestyle, including a balanced diet and regular exercise, can help manage weight and improve overall joint health.
- Medications: Over-the-counter pain relievers and prescription medications can provide relief from pain and inflammation associated with(OA).
- Physical Therapy: Tailored exercise programs designed by physical therapists can enhance joint flexibility, strengthen muscles, and improve overall joint function.
- Assistive Devices: Braces, canes, and orthopaedic footwear may be recommended to reduce joint stress and improve mobility, particularly in advanced cases.
- Surgical Interventions: In severe cases, surgical options such as joint replacement surgery can provide significant relief and improve the quality of life for those with advanced OA.
Is Osteoarthritis pain bearable?
OA pain can vary widely among individuals, with some experiencing mild discomfort and others enduring more severe pain. For many, OA pain is manageable through a combination of lifestyle modifications, pain relievers, and targeted therapies. Adopting a healthy lifestyle, maintaining a suitable weight, and engaging in low-impact exercises can significantly alleviate symptoms. Over-the-counter or prescription medications, such as acetaminophen or NSAIDs, can help manage pain and inflammation. While OA pain may be bearable for some, it is crucial for individuals to consult with Orthopedic doctor to develop a tailored treatment plan that addresses their specific needs and enhances their overall quality of life. Early intervention and a proactive approach to managing symptoms are key factors in successfully navigating(OA) pain.
How is arthritis differentiated from osteoarthritis
Arthritis is a comprehensive term encompassing diverse inflammatory joint conditions, and (OA) stands out as a specific subtype within this spectrum. While arthritis broadly denotes joint inflammation, various types exist, including rheumatoid arthritis (RA), psoriatic arthritis, and gout, among others. In contrast, OA is primarily a degenerative joint disease, distinct from autoimmune conditions. OA is characterised by the gradual breakdown of cartilage, commonly associated with ageing and joint wear and tear. Unlike inflammatory arthritis, OA is generally considered non-inflammatory, though mild inflammation may occur in later stages. Additionally, OA may affect joints unilaterally or asymmetrically, distinguishing it from certain autoimmune forms of arthritis that often manifest symmetrically. The differentiation involves a thorough examination of medical history, physical assessments, imaging studies, and sometimes blood tests to pinpoint the specific type of arthritis and guide appropriate management strategies.
Conclusion
In conclusion, Osteoarthritis (OA) is a challenging condition affecting numerous individuals, causing discomfort and hindering mobility. Dr. Hardik Padhiyar, an experienced orthopedic specialist, offers compassionate care and tailored treatment solutions to manage OA effectively, helping patients regain function and improve their overall quality of life.






